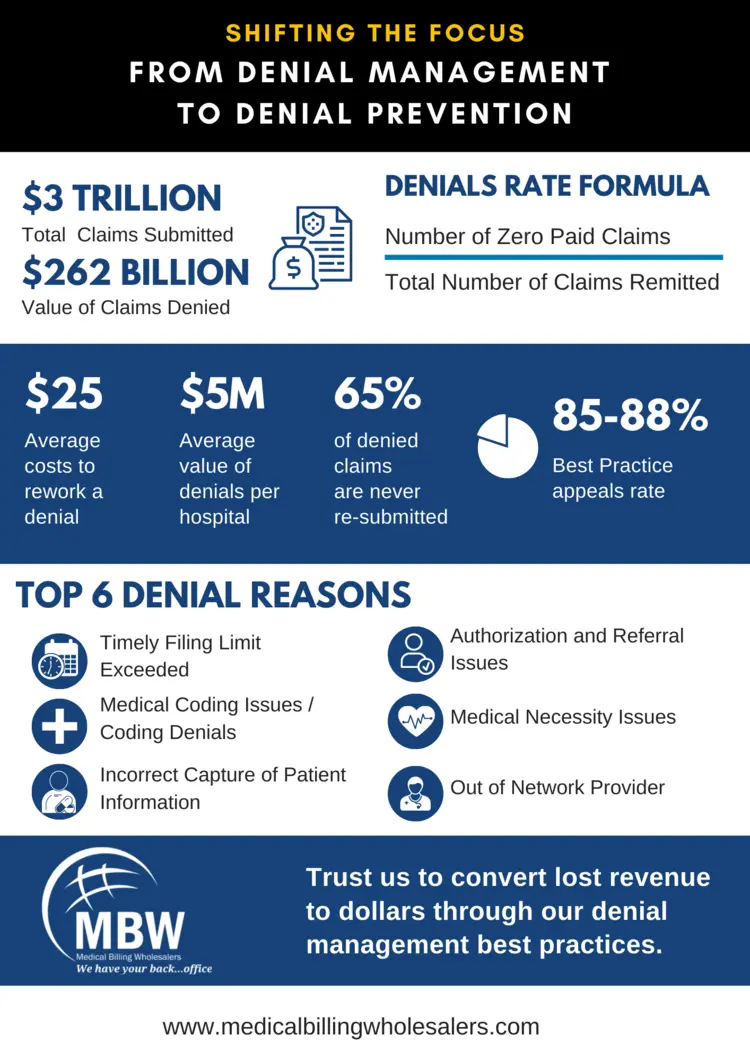
An overwhelming amount of time, money, and resources are spent by healthcare organizations to appeal denials. To understand the magnitude, look at these staggering numbers:
-
Of a total of $3 Trillion in healthcare claims, $262 Billion are denied.
-
With the amount of time addressing these denials takes, as many as 65% of these denied are never resubmitted
-
Denied claims can make a significant dent on an organization’s financial viability, and ineffective AR management is the #1 reason for the closure of a healthcare organization.
As revenue cycle administrators are caught in this vicious phase of managing denials, the resources that a denial prevention program seems like an additional burden on them. Contrary to this perception, denial prevention programs give you long-term and sustainable results and help you identify the root cause in each of the revenue cycle processes – Scheduling, patient registration, data capture quality, clinical documentation and coding, claims filing, and accounts receivable management.