Eligibility and Benefits Verification Services
Confirm eligibility and benefits, improve patient experience, and speed to care while improving collections.
Comprehensive Eligibility and Benefits Verification Services
Comprehensive Eligibility and Benefits Verification Services
In healthcare, it’s crucial for providers to confirm a patient’s eligibility and coverage for services before their appointment. This verification process is a key component in ensuring successful payment for services rendered. Statistics show that a major portion of denied claims, up to 75%, can be attributed to patients not being eligible for the services provided. Despite its importance, this process is often underemphasized in the healthcare revenue management cycle.
In healthcare, it’s crucial for providers to confirm a patient’s eligibility and coverage for services before their appointment. This verification process is a key component in ensuring successful payment for services rendered. Statistics show that a major portion of denied claims, up to 75%, can be attributed to patients not being eligible for the services provided. Despite its importance, this process is often underemphasized in the healthcare revenue management cycle.
Impact of Ineffective Eligibility and Benefits Verification:
When eligibility and benefits verification is not conducted effectively, it can lead to several negative outcomes:
- Increased Claim Denials: Unverified eligibility often results in denied claims because services are rendered to ineligible patients.
- Delayed Payments: Payment processes are slowed down, affecting the financial health of healthcare providers.
- Additional Rework: Inaccurate or incomplete verification necessitates extra administrative effort to rectify issues.
- Patient Care Delays: Patients may face delays in accessing needed care due to verification issues.
- Decreased Patient Satisfaction: Inadequate verification can lead to unexpected costs for patients, reducing their satisfaction.
By conducting comprehensive eligibility and benefits verification, we aim to streamline the revenue cycle for healthcare providers, enhancing both provider and patient experiences.
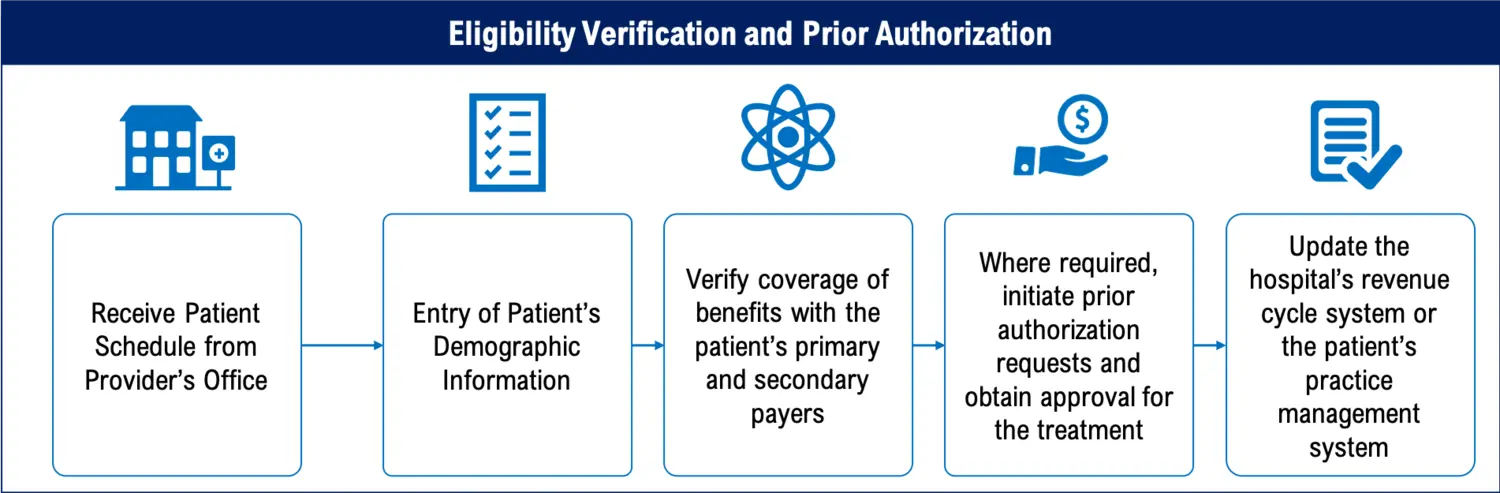
Our Approach to Eligibility Verification:
Patient Schedule Integration: Directly receiving patient schedules from the healthcare provider’s office, be it a hospital or a clinic, helps in planning and organizing the verification process efficiently.
Accurate Demographic Information Entry: Our team ensures precise entry of patient demographic details, which is fundamental in verifying eligibility and benefits correctly.
Comprehensive Coverage Verification and Benefit Analysis:
Navigating Insurance Complexities: We handle various complexities like dual eligibility, third-party eligibility, and out-of-state verifications.
In-Network and Out-of-Network Benefits: Determining whether the services are covered under in-network or out-of-network benefits, providing clarity on patient liability.
System Updates with Payer Details: After verifying eligibility, we update the hospital’s or practice’s revenue cycle system with all relevant payer details. This ensures that all the information is current and accurate.
Testimonials
Tennessee based Behavioral Health Billing Company
“I want to congratulate Medical Billing Wholesaler’s team for the way they handle every account. They take every step there is to take when a claim is denied for no authorizations, which includes going as far as re-verifying the benefits. The team does amazing work and we believe that is how it should be done!”
Ready to take your business to the next level?
Get in touch today and receive a complimentary consultation.
Our users are Happy & Healthy
Proficient FTE Handling
V.P.
Behavioral Collections Up by 50%
Dr. M.J.
Credentialing Simplified
K. W.
Lightning-Fast Support
Dr. H.N.
Proactive AR Management
Dr. S.L.
Finally Stress-Free
Dr. A.B.
Cardiology Denials Cut by 35%
Dr. T.L.
Healthcare partnerships

Effectively Combat Clinical Denials and Shift Focus to Denial Prevention
Benefits of Our Eligibility and Benefits Verification Services
Focus on Patient Care
By outsourcing eligibility verification to us, healthcare providers can prioritize patient care over administrative tasks. We reduce the workload on the healthcare provider’s staff and minimize errors and delays.
Improve Speed to Care
Efficient processing of eligibility requests accelerates scheduling for care reviews, leading to enhanced patient satisfaction and better physician utilization.
Reduce Claim Denials
By processing eligibility verifications efficiently, we reduce claim denials and accelerate cash flow.
Improve POS Collections
Upfront determination of Patient responsibility for payments reduces patient debts and improves POS collections, besides improving Patient Satisfaction
Expertise You can Trust
We work with all the major commercial and government healthcare payers including Blue Cross Blue Shield (BCBS), Aetna, Humana, United Healthcare, and others. Our team works with multiple medical specialties, across various states, and different size practices.
Cost Efficiency
In-house verification can be costly. Our team members based in India pick up the work queues and process each request diligently
Explore our Latest Thinking
Request for Information
Enhance your patient care by establishing a high-performance revenue cycle with our expertise in eligibility and benefits verification. Simply fill out the form below, and one of our specialists will promptly reach out to assist you.


