
Physician Credentialing and Enrollment Services
Reduce out-of-network denials. Improve speed-to-care.
Provider Credentialing and Enrollment Services
Physicians/providers must credential themselves, i.e., enroll and attest with the Payer’s network and authorized to provide services to patients who are members of the Payer’s plans. The credentialing process validates that a physician meets standards for delivering clinical care, wherein the Payer verifies the physician’s education, license, experience, certifications, affiliations, malpractice, any adverse clinical occurrences, and training.
Payers may delay or refuse payments to physicians who are not credentialed and enrolled with them. These impact the financials of the practice negatively. Our customized Payer credentialing and enrollment services support physicians in:
- Starting or joining a new practice
- Switching from one physician practice group to another
- Join or become affiliated to new groups or practices
- Enroll with new payers
- Maintain their credentialing services.

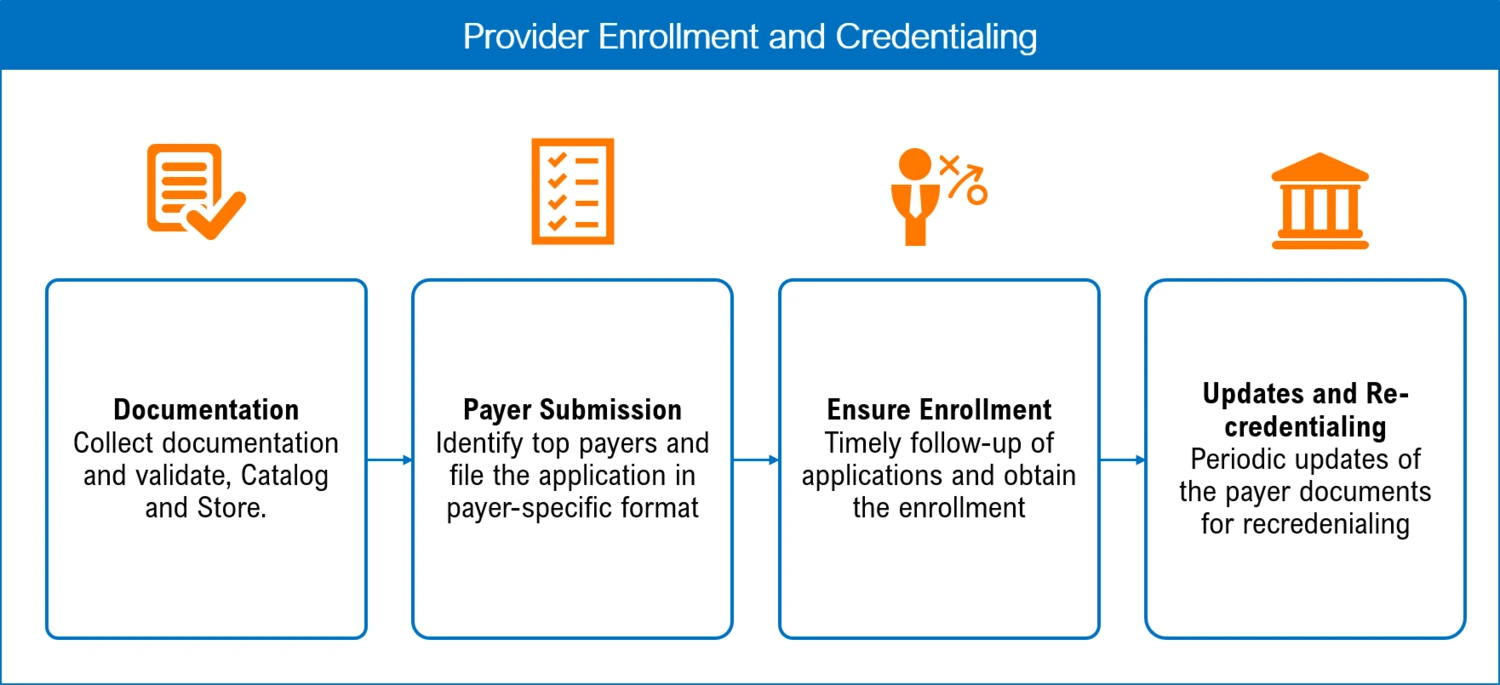
Our Credentialing Process Involves
- Collect all the data and documents required for filing credentialing applications from the physicians
- Store the documents centrally on our secure document management systems
- Understand the top payers to which the practice sends claim and initiate contact with the payers
- Apply the payer-specific formats after a due audit
- Timely follow-up with the Payer to track application status
- Obtain the enrollment number from the Payer and communicate the state of the application to the physician
- Periodic updates of the document library for credentialing purposes
Our Physician Credentialing Services Include:
New Registrations/Renewals of an Individual Provider
- With the State
- With the Drug Enforcement Agency (DEA)
- Provider Data Maintenance – Update Management on Payer Systems
- Provider demographic update in payers file. (Updates of Provider’s specialty or additional educational qualifications)
- Provider directory maintenance on payer websites. ( Checking payer website and verifying provider details like Phone and Fax #, Zip code. Updating the correction to payers )
- EFT/ERA enrollments
- Contracting Creation and Maintenance
- New Group/Individual Practitioner contracts
- Adding / Deleting providers in the existing contract
- Adding/Deleting location in the current contract
- Adding / Deleting plan types ( Line of Business ) in the current contract
- Rate Negotiation
- CAQH application filing
- CAQH quarterly attestations
-
Expirations and Renewals
- The tracking expiry date for State DEA License, Board certificate, and Malpractice Insurance
-
Tracking and Analytics
- Maintaining a repository of provider’s credentialing documents
- Maintaining Contracting agreements
- Tracking credentialing dates, expiration, and alerting dates to initiate credentialing processes
- Working with the denials team to understand if there are any claim denials due to credentialing issues
Texas based HealthCare Centre
“I wanted to thank the Medical Billing Wholesalers team for providing us assistance with our address change project. They are very responsive, attentive and proactive in resolving our concerns. Thanks to the MBW management for providing us amazing people to help at critical times in our practice evolution process-which I sincerely appreciate!”
Ready to take your business to the next level?
Get in touch today and receive a complimentary consultation.
Our users are Happy & Healthy
Proficient FTE Handling
V.P.
Behavioral Collections Up by 50%
Dr. M.J.
Credentialing Simplified
K. W.
Lightning-Fast Support
Dr. H.N.
Proactive AR Management
Dr. S.L.
Finally Stress-Free
Dr. A.B.
Cardiology Denials Cut by 35%
Dr. T.L.
Healthcare partnerships

Effectively Combat Clinical Denials and Shift Focus to Denial Prevention
Benefits of Our Provider Credentialing Services
Faster Provider Onboarding
Accelerates the process of integrating new providers into the network, leading to quicker service expansion and patient care delivery.
Expertise and Accurac
Leverage the expertise of specialists in credentialing, ensuring high accuracy and adherence to regulatory standards.
Continuous Monitoring and Updates
We offer ongoing monitoring and timely updates of provider credentials, maintaining the highest level of professionalism and care standards.
Time and Resource Efficiency
Outsourcing provider credentialing saves significant time and resources, allowing healthcare providers to focus more on patient care rather than administrative tasks.
Reduced Administrative Burden
Reduced Administrative Burden: Minimizes the workload on in-house staff, reducing administrative overhead and streamlining processes.
Compliance Assurance
Ensures compliance with all relevant healthcare regulations and standards, mitigating risk of non-compliance penalties.
Explore our Latest Thinking
Request for Information
Enhance our network’s proficiency and patient trust by partnering with us for streamlined provider credentialing and enrollment services. Simply fill out the form below, and one of our experts will quickly reach out to assist you.


