When billing for prolonged service, not only should you be aware of the guidelines from CMS but you should also ensure that the physicians and clinical staff are educated about the use of the right CPT codes.
ViewPoint
While the application of prolonged service codes may be reasonably straightforward, few codes cause more confusion than prolonged service codes. It may be noted that prolonged service codes can be used for outpatient procedures as well as for inpatient care. These codes are typically used to bill for services that significantly exceed the standard time a physician takes while providing care. These may include face-to-face services as well as non-face-to-face services.
While prolonged service coding issues are highlighted in this case study, the principles of educating physicians and clinical staff is applicable for all cases where coding denials are high.
Results Summary
Customer Situation
A New Jersey-based multi-specialty practice was getting a lot of denials for the prolonged service codes. The practice was billing office visit codes along with the prolonged service codes for the additional time spent with patients to monitor them post rendering of medical tests and procedures.
Claims for these procedures were denied as mutually exclusive service and the physician was concerned about not getting paid for these billed CPT codes
Challenges with Prolonged Service Claims
Specifically, a new physician who has joined the practice was spending additional time with patients after Esketamine Drug to monitor their response. He would apply the codes 99358 & 99359 for the prolonged services along with outpatient visit code. These claims were getting denied as 99358 & 99359 were considered mutually exclusive.
What is prolonged service?
A physician when spending additional time to the patients for any services that are not billable by a separate CPT code can use prolonged service codes. Prolonged service CPT codes are 99354 – 99359. CPT 99354 to 99357 used for face to face service and 99358 to 99359 used for non-face to face service..
Solution
The direct, prolonged service Current Procedural Terminology (CPT®) codes (99354-99357) can be used when a physician or other qualified healthcare professional provides prolonged service in an inpatient or outpatient setting. The prolonged service is a service that goes beyond the usual service duration described for the E/M code.
Medical Billing Wholesalers’ denial management team identified the issue and asked the Coding team to look into it. Our team looked at the CMS guidelines and found that:
- CPT 99358 & 99359 should not be billed with an office visit code since it should be charged for non-face to face service only.
- CPT 99354 to 99357 must be charged with an office visit code since all these codes are add-on codes.
Having identified the issue, we documented our findings and explained the right codes to be used to the Physician. As a practice, we asked them to release the superbill with these codes for prolonged service going forward.
Results
Not only were we able to resolve the claims but also educate the practice’ team on the usage of the right CPT codes for prolonged service.
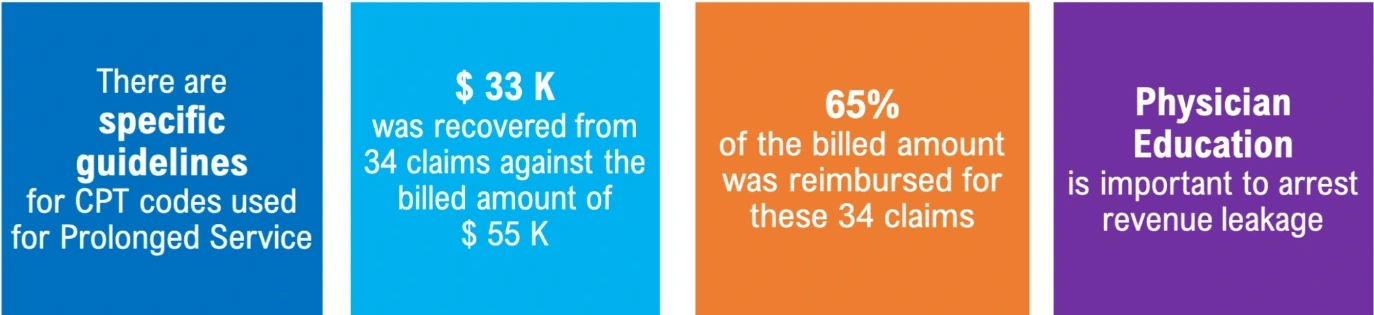
- A total of 34 claims with a charged amount adding up to $ 51 K had been denied. These claims were re-submitted, and approximately $33K was reimbursed, i.e., 65% of the billed amount.
- Our team identified the issue during the first month of occurrence, and we were able to set preventive guidelines before it affected more claims. The Physician is now regularly reimbursed for prolonged service claims.





