Correct Coding and Re-submission of Pain Management Claims help Recover $300K of A/R Backlog
Standardized billing and coding practices for Spinal Cord Stimulator (SCS) Procedure Code 63650 reduce medical necessity denials and help collect 281 claims valued over $ 300K in 2 years.
Viewpoint:
With ever-increasing complexities of revenue cycle management processes, accounts receivable backlogs are relatively common. Working denied claims requires expertise to uncover the reasons for the denials and a maniacal pursuit of potential solutions. A strong collaboration between your medical coding and denial management teams can often provide the answers and help you resolve claims worth millions of dollars. A strong understanding of the provider’s medical specialty, common reasons for denials, and the understanding of the filing requirements different payers do accelerate your revenue cycle.
Results Summary
Customer Situation
A Portland-based Pain Management Clinic was receiving a lot of denials for claims relating to the Spinal Cord Stimulator procedure. Upon Initial analysis, the claims had been coded correctly. However, the impact of these claims was huge. The source of the denials had to be nailed to resolve the unpaid claims.
Understanding the procedure – Spinal Cord Stimulator
Billed using the CPT code 63650, the procedure involves the insertion of two needles into Spinal Epidural Space. Each needle should be considered as one unit, and each unit needs to be billed as a separate line item along with a supportive modifier to get both units paid. Spinal Cord Stimulator is a high-dollar value procedure in Pain Management. The physician will consider this procedure only when the patient is continuing to suffer from chronic pain even after other treatments such as medication and physiotherapy. As a specialized pain management clinic, the provider saw a high rate of denials on account of these specific eligibility requirements. CMS established non-facility practice expense (PE) relative value units (RVUs) for CPT 63650 that are valued to include payment for the lead(s) and other practice expenses associated with office-based trials. The guidelines mandate that the patient should undergo a Psychiatric Evaluation test to ascertain the medical necessity for the procedure. However, these coding guidelines were not well understood by the clinic’s in-house team.
Solution
SCS Trial Billed vs Denied comparison for seven months before and after the issue was fixed
A few months after the successful transition of the processes to our offshore teams, we noticed that the claims relating to the Spinal Cord Stimulator procedure were getting consistently denied and started exploring for a solution.
The encounter was created by appending modifier “51 -multiple surgeries/procedures” on second line items or combination of modifier 51 & 76 on both line items, respectively. However, the Payer paid for one unit and denied the second unit as inclusive.
We identified this issue, reviewed detailed billing guidelines, and tried rebilling denied claims by appending modifier 76 only to the second line item. Insurance reprocessed the claim and paid for the second unit of service.
We worked with the Physician’s office and educated them on the need to append modifier 76 to the second line item. In case, the Payer requests for additional information, medical records including operative reports, history of the condition, Psychiatric Evaluation notes should be provided to ensure that the medical necessity of the procedure is justified.
Result:
Improvement in Receivables
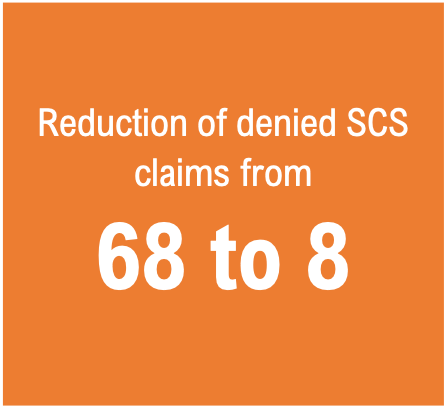
Reduction in the no. of SCS denied claims. Since the identification of the issue in Jun 2017, we were able to develop and institutionalize the solution by the beginning of 2018 using subsequent re-filing of the claims
From as many as 68 claims being denied in the second half of 2017, we were able to reduce the denied claims to 8 in the first half of 2018.
Resolved the Inclusive Procedure Denials. None of the claims are getting denied for procedure code 63650 as inclusive. It reduced the denials ratio tremendously in overall practice performance.
Cleared A/R Backlog. We cleared all the denied/AR pending claims affected due to this issue and received a payment of around $90K.
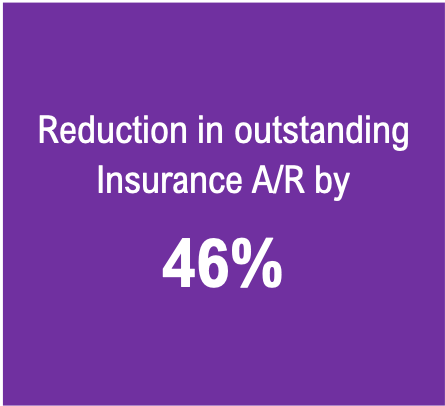
~50% Reduction in Insurance A/R. Through consistent follow-up, root cause analysis of each denied claim, and systemically addressing each issue, we were able to reduce the overall Insurance A/R from $ 1.1 M to less than $ 600K in two years.
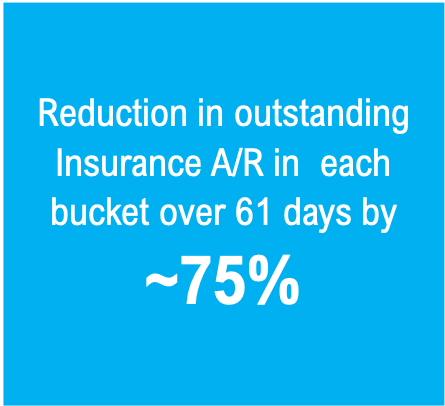
Keeping A/R Current. By September 2019, we reduced the A/R in the >60-day buckets, i.e. 61-90, 91-120, and 121+ day buckets, to a quarter of the June 2017 numbers
Improvement in Practice Collections. Improved the average monthly collection of the practice from by 36% from $170K to $231 K.
Impact on A/R
Request for Information
Facing issues with backlogged A/R, we can help. Please fill the form below to schedule a no-obligations discussion on how we can help you resolve your A/R issues and achieve industry’s leading benchmarks.