Case Study: Improved Revenue Cycle Workflow and reporting functionality accelerates Cash Flow
Most revenue cycle systems have a wealth of unutilized functionality. Revenue cycle professionals need to evaluate workflow and reporting functionality on the revenue cycle system to not only ease their workload but also improve revenue cycle outcomes
ViewPoint
A revenue cycle system is only as good as its implementation. The very premise of software programs is to reduce human effort. Yet most revenue cycle professionals utilize less than half of the capabilities of the system. Important functionalities that can reduce workload significantly are often overlooked. Revenue Cycle Professionals should look at their workload as well as performance data to understand how they can ease their work processes and exceed benchmark KPIs, by taking advantage of dormant features of the revenue cycle platform.
Results Summary
Customer Situation
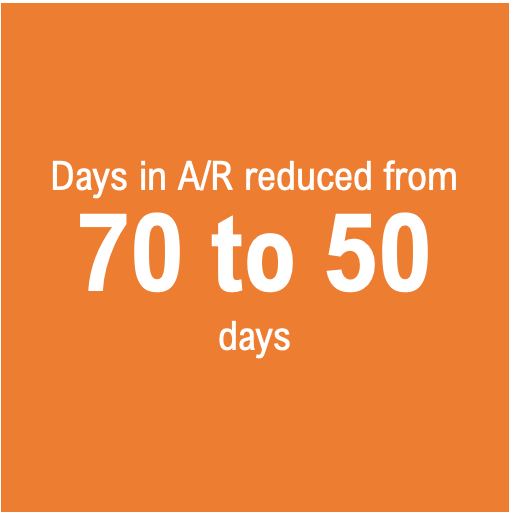
An Illinois based Pathology group addressing clinical & anatomic pathology group was in a significant backlog situation with its revenue cycle. Pile up demographic data capture and charge entry, and delayed claims submission was leading to an increased number of days in A/R, often over 70 days.
Challenges
When Medical Billing Wholesalers was presented with this set of problems during transition, we set up a cross-functional team of billers, coders, and IT team members from our side. Each of our team members was required to catalog the issues and bring it up for a discussion each week so that the aggregated set of issues could be addressed systematically. Broadly, we identified issues in the following areas:
System Related issues
Delays in receiving demographic and charge data from the practice as the communication workflow did not have clear work queue definition and alerting mechanism
The system was not configured to check for duplicate charges. Hence, for each patient, the recent charges had to be manually checked, which added to the time taken to enter charges
The system’s layout was not intuitive for performing billing tasks. Lack of intuitive interfaces and often redundant work added to the time taken to process.
There were frequent outages and latency issues were common. Hence, there was a need to evaluate the connectivity as well as server infrastructure.
Coordination issues between the front office and the billing team
The front office team did not capture the demographic information on time and hence the charge volume constantly fluctuated, often, needing additional staff deployment to address the backlog.
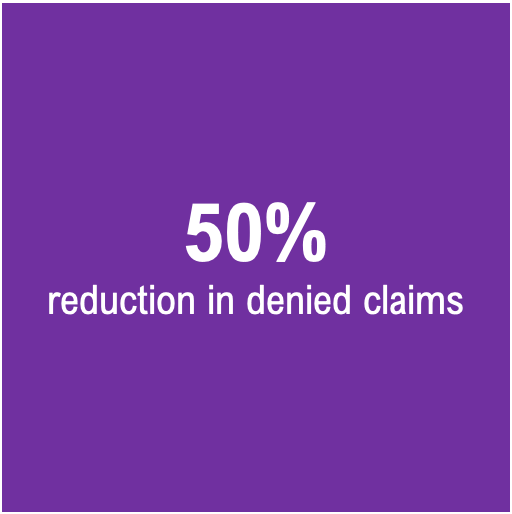
Timely filing issues and A/R backlog
The cascading impact of the delays in front-end processes led to an increase in AR days to over 70 days, erratic monthly collections, and a high percentage of denied claims for timely filing limit being exceeded.
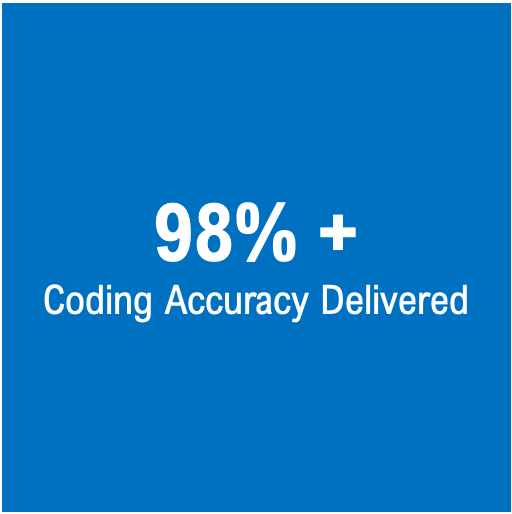
Coding Accuracy
Lack of appropriate information leading to coding accuracy issues.
Solution
With clear identification of the issues, the Medical Billing Wholesalers team improved revenue cycle KPIs of the client by:
Addressing System Issues
Worked with the Practice’s team to streamline billing interfaces and added a feature to catch duplicate charges.
Work closely with our client’s IT team and fixed the connectivity and slowness issue.
Reducing Charge Entry Lag
Monitored charge queues to initiate follow-up with the front office team to obtain demographic information on time and enter charges on time
Sensitized the client’s leadership team and the front-office team on the delays in turning around demographic information and the impact it was having on their financial health
Improved Clean claims submission adhering to timely filing.
With charge entry lag being reduced, our team was able to enter charges on time, audit claims before submission, and adhere to timely filing requirements.
We also checked for eligibility with the insurance companies and followed up with patients to obtain accurate insurance information.
Improving Coding accuracy
Deployed specialty-specific coders to improve coding quality
Result
We were able to deliver the following results:
Days in AR reduced to less than 50 days
Timely filing denials were eliminated and as such denials were reduced by 50%
Charge entry backlog cleared, and situations of new backlog avoided
Use of certified coders improved coding accuracy to over 98%
Improved billing system functionality reduced the effort required to post charges
Reporting functionality was streamlined. A reporting cadence of weekly, monthly and quarterly reports was implemented to ensure that revenue cycle managers take timely decisions.
System availability and connectivity improved to over 99.9%
Reduced latency resulted in better productivity
Schedule a consultation
Our focus on resolving denials by identifying and systemically eliminate the root causes, helps our clients improve revenue by a minimum of 20%. To learn about how we can help you reduce denials and improve revenue cycle metrics, please fill the form below, and we will be in touch.